Do you think health care workers are often tested for coronavirus? Think Again: NPR

A nurse wears personal protective equipment as she prepares to treat a COVID-19 patient last month at a Missouri rural hospital.
Jeff Roberson / AP
Hide the caption
Toggle caption
Jeff Roberson / AP

A nurse wears personal protective equipment as she prepares to treat a COVID-19 patient last month at a Missouri rural hospital.
Jeff Roberson / AP
At a recent roundtable with Joe Biden, nurse Mary Turner Tell The president-elect is something he found surprising:
“Did you know that I haven’t tried yet?” Turner, who is the chief, said Minnesota Nurses Association. “And I’ve been on the front lines of the ICU since February.”
“You are kidding me!” Biden responded.
You are not kidding.
Guidance from the Centers for Disease Control and Prevention indicates this Healthcare personnel are tested If they have symptoms or have known exposure to the Coronavirus. But treating COVID-19 patients while wearing personal protective equipment is not an exposure that warrants testing.
Recent survey by United National Nurses, Which is the largest association of registered nurses in the country, have found Only 42% of RNs in hospitals said they had been tested for the virus.
He said, “It still amazes me that we don’t do that.” Michael Mina, An epidemiologist at the Harvard TH Chan School of Public Health. While personal protective equipment goes a long way toward protecting health care workers, he says, outbreaks have occurred in hospitals.
At Brigham and Women’s Hospital in Boston, where Mina runs the virology lab, The outbreak this fall It affected 42 employees and 15 patients. The hospital said that the factors that led to the outbreak include patients not wearing masks, staff not wearing eye protection, and employees’ failure to distance themselves from social distances while eating.
But Mina believes that with more tests, the virus will not spread widely.
“This is an outbreak that shouldn’t have happened. I firmly believe we wouldn’t have seen an outbreak increase so quickly – and we wouldn’t be able to start if we were running repeated tests.”
hazard identification
Mina said Imagine doctors in a hospital infected with the virus but not showing symptoms. Doctors are not aware that they have been exposed to the infection and now operate and are more contagious.
“They pose a very serious danger,” Mina said. “At some point in the day, you take off your mask for lunch. If you are having lunch in a cafeteria, you may reveal 10 people without even knowing it – especially in a hospital setting where you can have vulnerable people all around.”
Ideally, he said, people wear masks and socialize. But especially with winter coming, more things will happen indoors. “People will have to eat. Whether it’s in the break room or the cafeteria, you really risk putting others at risk.”
Nancy Foster American Hospital AssociationThe vice head of quality policy and patient safety, said hospitals are following the CDC’s scientific guidelines.
“These strategies were implemented in the early days of the pandemic, when there were persistent concerns about shortages of test kits and supplies. Hospital and CDC staff did not want to divert available test supplies away from patients and the general population,” Foster said in a statement to NPR, adding The American Heart Association continues to urge the federal government to increase the supply of personal protective equipment and test supplies.
Maggie McGillick, spokeswoman American College of Emergency PhysiciansSword masks and personal protective equipment provide strong protection.

Nurses helped a patient from COVID-19 last month at a Los Angeles hospital. The California Department of Public Health now strongly recommends that hospitals test all their healthcare personnel for the coronavirus every week.
Jae Se Hong / AP
Hide the caption
Toggle caption
Jae Se Hong / AP

Nurses helped a patient from COVID-19 last month at a Los Angeles hospital. The California Department of Public Health now strongly recommends that hospitals test all their healthcare personnel for the coronavirus every week.
Jae Se Hong / AP
“It is almost impossible to transmit the virus through an N95 mask. [powered air purifying respirators]Or other devices, “as I wrote in an email to NPR.” Those who do not have close contact routinely wear masks. Hand washing and using gloves is part of their routine, so it is extremely rare for an infected healthcare professional to transmit the disease to anyone at work. “
‘Precautions and personal protective equipment work’
Just like other Americans, many healthcare workers contract the virus across society. Last month, the Mayo Clinic said so More than 900 employees In Minnesota and Wisconsin, I have gotten COVID-19 in the past two weeks, out of 55,000 employees there.
The main source of exposure for infected employees is known exposure to someone in the home, said Laura Briher, Medical Director of Occupational Health at Mayo Clinic.
How does the clinic know that the virus does not spread between workers?
“We are tracking the source of the infection very carefully,” said Priher – she said that the infection rate for healthcare workers in the clinic who work on campus in patient care roles is similar to the infection rate for on-campus employees who do not work with patients and those who are work from home.
“It is very reassuring to us that precautions and PPE are working,” said Priher.
Many hospitals are now requiring patients to take a negative test for coronavirus in the few days before an inpatient procedure. Meanwhile, doctors and nurses themselves are unlikely to get tested before their procedure.
Why are the criteria different?
The reason for this, Briher said, is because in many procedures, patients cannot be hidden.
She said that many patients “need procedures that increase the risks, such as the use of continuous positive pressure devices in the airways.” At night or things like that. So we want to make sure we keep our healthcare campus as safe as possible. ”
Screening of healthcare workers on a large scale
There are methods that hospitals can use to regularly test large numbers of health care workers – either by using rapid antigen tests or by pooling polymerase chain reaction tests, said Mina, a Harvard epidemiologist.
“They can take a swab from everyone, put 50 swabs at a time in one tube, run that one tube and collect tests for a very cheap cost. You can do whole hospital departments with one test for $ 50 a day,” he says. If the pool test results are positive, the hospital can return and individually test the people in it to see who has the virus.
And fast Antigen tests It can work better: “They only discover people when they are contagious.”
This could make antigen tests an ideal option for screening purposes, Mina said, because some people continue to test positive for PCR tests for several weeks after they stop the infection. This could help hospitals that are already understaffed.
“Lots of people are contagious, for example, for only four days. So maybe [with antigen testing] You are back at work two days after being negative. Isolation may only last for five or six days. “
In California, new guidelines “strongly recommend” weekly testing
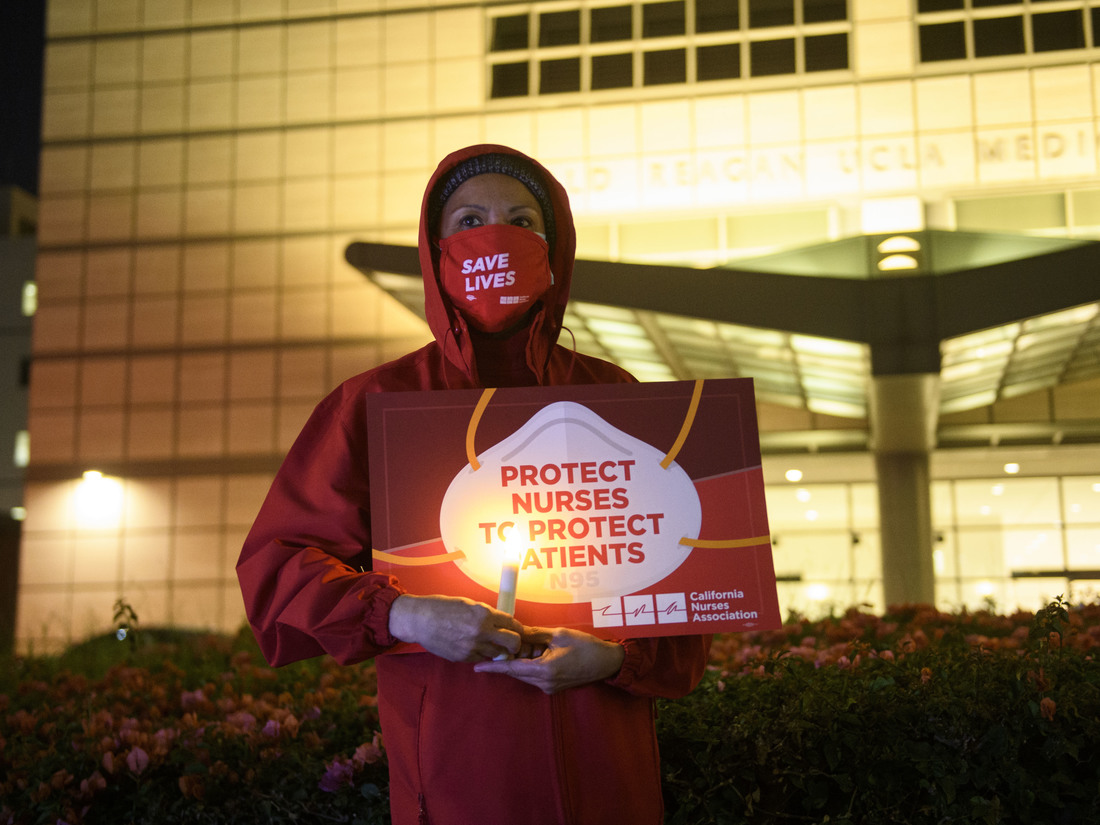
A nurse holds a candle during a protest in Los Angeles last month for healthcare workers who died from COVID-19.
Patrick T. Fallon / AFP via Getty Images
Hide the caption
Toggle caption
Patrick T. Fallon / AFP via Getty Images

A nurse holds a candle during a protest in Los Angeles last month for healthcare workers who died from COVID-19.
Patrick T. Fallon / AFP via Getty Images
California Department of Health announced New tips Two weeks ago, I strongly recommended hospitals to have weekly testing for health care personnel – and he suggested that combined testing might be a way to do so.
But Susan Butler WuThe state’s new recommendations will be difficult for most hospital laboratories to implement, said an assistant professor of clinical pathology at the University of Southern California and director of the Clinical Microbiology Laboratory at a large hospital in Los Angeles.
At her private hospital, she estimated that 10,000 people would need a weekly exam. Without operational support from the state, I anticipated the new protocols would cause problems – including further delays in testing.
Butler-Wu said, “When you get a big mandate, ‘Hey, test all the healthcare workers in your hospital,’ I don’t have a bunch of fairies with magic wipes and magic reagents that are going to magically run this.
Butler-Wu said the guidelines could also lead to staff shortages, if employees who recently had COVID-19 suddenly without positive symptoms get PCR tests.
They may not be infectious anymore, she said, “But what do we do now? We tell them to isolate. Now we lose a whole bunch of employees as a result.” “We are asking people to stay home and not work when they are really necessary and may not pose an infectious risk to anyone.”
The biggest problem, Butler Wu said, is a systemic problem.
“As a country, because we do not have a national plan or a national strategy, this is the situation in which we find ourselves: soccer players can take the tests,” she said. “People who choose to socialize with others and want to feel safe doing it, even though it’s a pandemic, can take the tests.”
But a national program to regularly test health care workers in the country? There is no one.
Anne Jackson is a nurse in the University of Michigan Health System. She said it was frustrating to read about the state of football players and coaches at the university Tested dailyHospital personnel are only tested if they have symptoms or have a CDC-specific exposure. (The university also has an open monitoring test program for employees who want to test.)
“Football makes them money,” Jackson said. “Health system employees do as well, but not to the extent that footballers do, and footballers are more valuable to them than we are.”
For Mina, a Harvard epidemiologist, the lack of regular testing for health-care workers raises other questions.
Mina said, “There is a clear problem when we say that the people who are most at risk, and the people most at risk to themselves and their patients are health care workers.” “That’s why we’ll give them vaccinations before everyone else. But then when we don’t have a vaccine, and it’s just a test, we say,” Don’t worry about that, it’s not a big problem, you don’t need to get tested. “
It is an approach, This is illogical, he said.
Will Stone contributed to this report.

Communicator. Reader. Hipster-friendly introvert. General zombie specialist. Tv trailblazer






